Rheumatoid arthritis

CHIDAMBARAM HOSPITALचिदंबरम अस्पताल,ചിദംബരം ഹോസ്പിറ്റൽ
சிதம்பரம் மருத்துவமனை,திசையன்விளை.627657
Dr.M.I. கிறிஸ்டோபர் சாமுவேல் MBBS,MS.,FIAGES.,லேப்ராஸ்கோப்பி அறுவை சிகிச்சை நிபுணர்.,
DR.அலெக்ஸ் J கிறிஸ்டோபர் MBBS,MS,MCH.,(PAEDIATRIC SURGEON),லேப்ராஸ்கோப்பி அறுவை சிகிச்சை நிபுணர்.,
DR.அருண் G கிறிஸ்டோபர் MBBS,MD(Anaesthesia)மயக்க மருந்து நிபுணர்,Pain Management., Dip.Diab., சர்க்கரை வியாதி மருத்துவர்.,
PT.அந்தோணி றீகன் B.P.T
(பிசியோதெரபி நிபுணர்)MCSE,COPA,D.Pharm., DR.அலெக்ஸ் J கிறிஸ்டோபர் MBBS,MS,MCH.,(PAEDIATRIC SURGEON),லேப்ராஸ்கோப்பி அறுவை சிகிச்சை நிபுணர்.,
DR.அருண் G கிறிஸ்டோபர் MBBS,MD(Anaesthesia)மயக்க மருந்து நிபுணர்,Pain Management., Dip.Diab., சர்க்கரை வியாதி மருத்துவர்.,
PT.அந்தோணி றீகன் B.P.T
Rheumatoid arthritis
Also called: RA, atrophic arthritis
A chronic inflammatory disorder affecting many joints, including those in the hands and feet.
Common
More than 1 million cases per year (India)
Can't be cured, but treatment may help Requires a medical diagnosis
Lab tests or imaging always required Chronic: can last for years or be lifelong
In rheumatoid arthritis, the body's immune system attacks its own tissue, including joints. In severe cases, it attacks internal organs.
Rheumatoid arthritis affects joint linings, causing painful swelling. Over long periods of time, the inflammation associated with rheumatoid arthritis can cause bone erosion and joint deformity.
While there's no cure for rheumatoid arthritis, physiotherapy and medication can help slow the disease's progression. Mild cases can be managed with anti-inflammatory medication (NSAIDs). More severe cases can be managed with a class of medications called anti-rheumatic drugs (DMARDS).
Symptoms
Signs and symptoms of rheumatoid arthritis may include:
- Tender, warm, swollen joints
- Joint stiffness that is usually worse in the mornings and after inactivity
- Fatigue, fever and weight loss
Early rheumatoid arthritis tends to affect your smaller joints first — particularly the joints that attach your fingers to your hands and your toes to your feet.
As the disease progresses, symptoms often spread to the wrists, knees, ankles, elbows, hips and shoulders. In most cases, symptoms occur in the same joints on both sides of your body.
About 40 percent of the people who have rheumatoid arthritis also experience signs and symptoms that don't involve the joints. Rheumatoid arthritis can affect many nonjoint structures, including:
- Skin
- Eyes
- Lungs
- Heart
- Kidneys
- Salivary glands
- Nerve tissue
- Bone marrow
- Blood vessels
Rheumatoid arthritis signs and symptoms may vary in severity and may even come and go. Periods of increased disease activity, called flares, alternate with periods of relative remission — when the swelling and pain fade or disappear. Over time, rheumatoid arthritis can cause joints to deform and shift out of place.
SymptomsRequires a medical diagnosisRheumatoid arthritis affects joint linings, causing painful swelling. Over long periods of time, the inflammation associated with rheumatoid arthritis can cause bone erosion and joint deformity.
People may experience:
Pain areas: in the back, joints, or muscles
Joints: stiffness, swelling, tenderness, or weakness
Whole body: anaemia, fatigue, or malaise
Skin: lumps or redness
Hand: bump on the finger or swelling
Also common: dry mouth, flare, physical deformity, or sensation of pins and needles
Causes
-
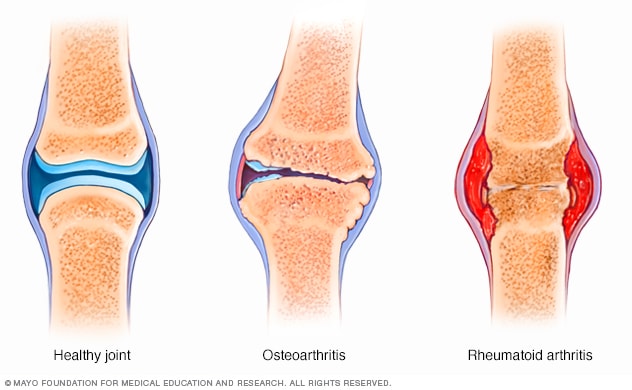
Rheumatoid arthritis vs. osteoarthritis
Rheumatoid arthritis occurs when your immune system attacks the synovium — the lining of the membranes that surround your joints.
The resulting inflammation thickens the synovium, which can eventually destroy the cartilage and bone within the joint.
The tendons and ligaments that hold the joint together weaken and stretch. Gradually, the joint loses its shape and alignment.
Doctors don't know what starts this process, although a genetic component appears likely. While your genes don't actually cause rheumatoid arthritis, they can make you more susceptible to environmental factors — such as infection with certain viruses and bacteria — that may trigger the disease.
Risk factors
Factors that may increase your risk of rheumatoid arthritis include:
- Your sex. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Family history. If a member of your family has rheumatoid arthritis, you may have an increased risk of the disease.
- Smoking. Cigarette smoking increases your risk of developing rheumatoid arthritis, particularly if you have a genetic predisposition for developing the disease. Smoking also appears to be associated with greater disease severity.
- Environmental exposures. Although uncertain and poorly understood, some exposures such as asbestos or silica may increase the risk for developing rheumatoid arthritis. Emergency workers exposed to dust from the collapse of the World Trade Center are at higher risk of autoimmune diseases such as rheumatoid arthritis.
- Obesity. People who are overweight or obese appear to be at somewhat higher risk of developing rheumatoid arthritis, especially in women diagnosed with the disease when they were 55 or younger.
Complications
Rheumatoid arthritis increases your risk of developing:
- Osteoporosis. Rheumatoid arthritis itself, along with some medications used for treating rheumatoid arthritis, can increase your risk of osteoporosis — a condition that weakens your bones and makes them more prone to fracture.
- Rheumatoid nodules. These firm bumps of tissue most commonly form around pressure points, such as the elbows. However, these nodules can form anywhere in the body, including the lungs.
- Dry eyes and mouth. People who have rheumatoid arthritis are much more likely to experience Sjogren's syndrome, a disorder that decreases the amount of moisture in your eyes and mouth.
- Infections. The disease itself and many of the medications used to combat rheumatoid arthritis can impair the immune system, leading to increased infections.
- Abnormal body composition. The proportion of fat compared to lean mass is often higher in people who have rheumatoid arthritis, even in people who have a normal body mass index (BMI).
- Carpal tunnel syndrome. If rheumatoid arthritis affects your wrists, the inflammation can compress the nerve that serves most of your hand and fingers.
- Heart problems. Rheumatoid arthritis can increase your risk of hardened and blocked arteries, as well as inflammation of the sac that encloses your heart.
- Lung disease. People with rheumatoid arthritis have an increased risk of inflammation and scarring of the lung tissues, which can lead to progressive shortness of breath.
- Lymphoma. Rheumatoid arthritis increases the risk of lymphoma, a group of blood cancers that develop in the lymph system.
Diagnosis
Rheumatoid arthritis can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis.
During the physical exam, your doctor will check your joints for swelling, redness and warmth. He or she may also check your reflexes and muscle strength.
Blood tests
People with rheumatoid arthritis often have an elevated erythrocyte sedimentation rate (ESR, or sed rate) or C-reactive protein (CRP), which may indicate the presence of an inflammatory process in the body. Other common blood tests look for rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) antibodies.
Imaging tests
Your doctor may recommend X-rays to help track the progression of rheumatoid arthritis in your joints over time. MRI and ultrasound tests can help your doctor judge the severity of the disease in your bodyWhen to see a doctor
Treatment
There is no cure for rheumatoid arthritis. But recent discoveries indicate that remission of symptoms is more likely when treatment begins early with strong medications known as disease-modifying antirheumatic drugs (DMARDs).
Medications
The types of medications recommended by your doctor will depend on the severity of your symptoms and how long you've had rheumatoid arthritis.
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Over-the-counter NSAIDs include ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve). Stronger NSAIDs are available by prescription. Side effects may include ringing in your ears, stomach irritation, heart problems, and liver and kidney damage.
- Steroids. Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage. Side effects may include thinning of bones, weight gain and diabetes. Doctors often prescribe a corticosteroid to relieve acute symptoms, with the goal of gradually tapering off the medication.
- Disease-modifying antirheumatic drugs (DMARDs). These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate (Trexall, Otrexup, Rasuvo), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine).Side effects vary but may include liver damage, bone marrow suppression and severe lung infections.
- Biologic agents. Also known as biologic response modifiers, this newer class of DMARDs includes abatacept (Orencia), adalimumab (Humira), anakinra (Kineret), certolizumab (Cimzia), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), rituximab (Rituxan), tocilizumab (Actemra) and tofacitinib (Xeljanz).These drugs can target parts of the immune system that trigger inflammation that causes joint and tissue damage. These types of drugs also increase the risk of infections.Biologic DMARDs are usually most effective when paired with a nonbiologic DMARD, such as methotrexate.
Therapy
Your doctor may send you to a physical or occupational therapist who can teach you exercises to help keep your joints flexible. The therapist may also suggest new ways to do daily tasks, which will be easier on your joints. For example, if your fingers are sore, you may want to pick up an object using your forearms.
Assistive devices can make it easier to avoid stressing your painful joints. For instance, a kitchen knife equipped with a saw handle helps protect your finger and wrist joints. Certain tools, such as buttonhooks, can make it easier to get dressed. Catalogs and medical supply stores are good places to look for ideas.
Surgery
If medications fail to prevent or slow joint damage, you and your doctor may consider surgery to repair damaged joints. Surgery may help restore your ability to use your joint. It can also reduce pain and correct deformities.
Rheumatoid arthritis surgery may involve one or more of the following procedures:
- Synovectomy. Surgery to remove the inflamed synovium (lining of the joint). Synovectomy can be performed on knees, elbows, wrists, fingers and hips.
- Tendon repair. Inflammation and joint damage may cause tendons around your joint to loosen or rupture. Your surgeon may be able to repair the tendons around your joint.
- Joint fusion. Surgically fusing a joint may be recommended to stabilize or realign a joint and for pain relief when a joint replacement isn't an option.
- Total joint replacement. During joint replacement surgery, your surgeon removes the damaged parts of your joint and inserts a prosthesis made of metal and plastic.
Surgery carries a risk of bleeding, infection and pain. Discuss the benefits and risks with your doctor.
Alternative medicine
Some common complementary and alternative treatments that have shown promise for rheumatoid arthritis include:
- Fish oil. Some preliminary studies have found that fish oil supplements may reduce rheumatoid arthritis pain and stiffness. Side effects can include nausea, belching and a fishy taste in the mouth. Fish oil can interfere with medications, so check with your doctor first.
- Plant oils. The seeds of evening primrose, borage and black currant contain a type of fatty acid that may help with rheumatoid arthritis pain and morning stiffness. Side effects may include nausea, diarrhea and gas. Some plant oils can cause liver damage or interfere with medications, so check with your doctor first.
- Tai chi. This movement therapy involves gentle exercises and stretches combined with deep breathing. Many people use tai chi to relieve stress in their lives. Small studies have found that tai chi may reduce rheumatoid arthritis pain. When led by a knowledgeable instructor, tai chi is safe. But don't do any moves that cause pain.
Make an appointment with your doctor if you have persistent discomfort and swelling in your joints.